Ketamine for Chronic Pain Management: Does It Really Work?
Chronic pain affects millions of Australians, and with growing frustration around conventional treatments, many people are turning toward newer therapies such as ketamine for pain management. While ketamine has gained popularity in clinical settings—particularly for acute or postoperative situations—there is still no strong evidence supporting its long-term effectiveness for chronic pain.
More importantly, ketamine does not address the root cause of pain. Instead, it temporarily alters how the brain perceives pain signals. Functional Patterns offers an alternative—one that focuses on correcting the biomechanical dysfunctions that actually create pain in the first place.
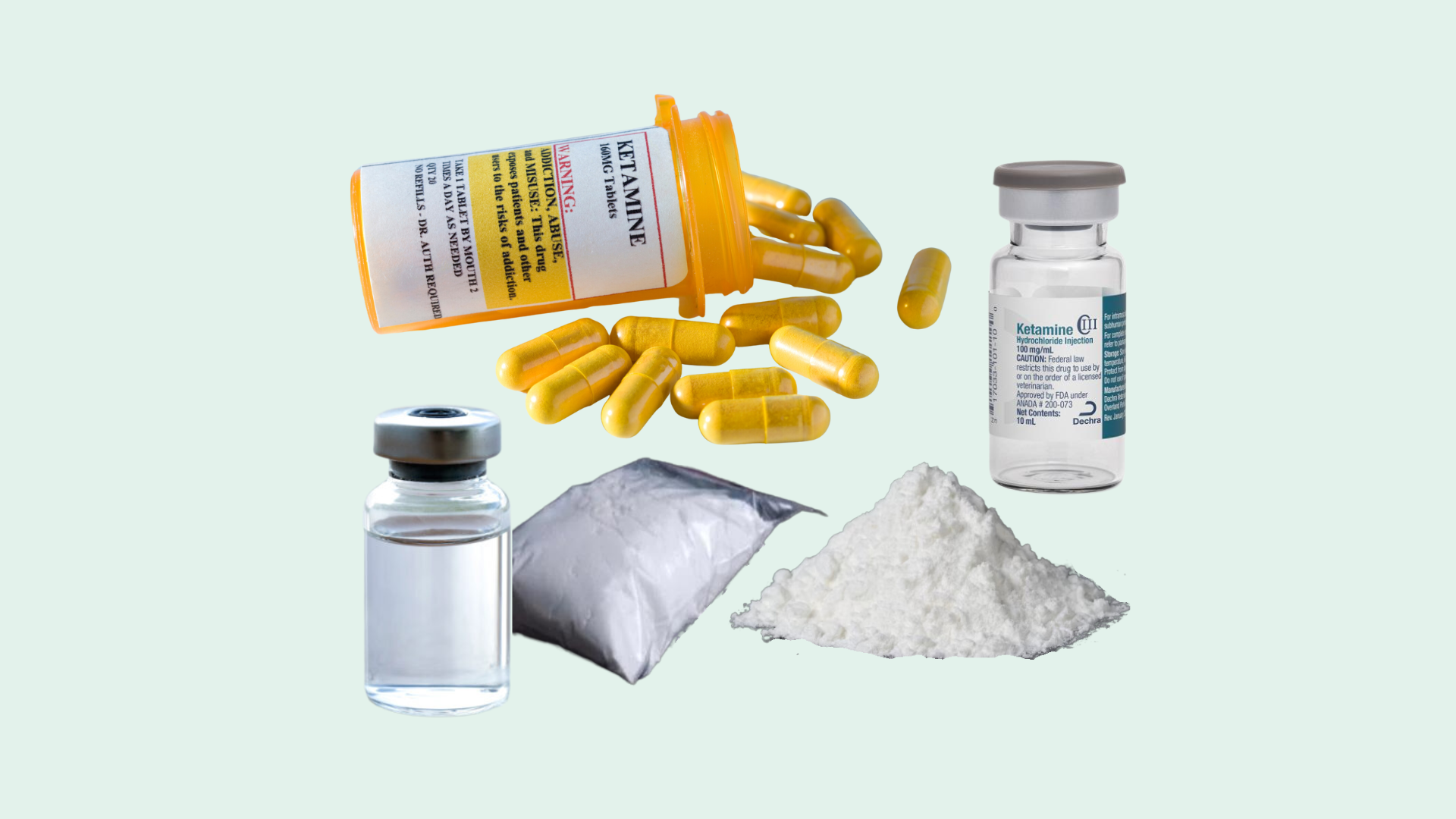
What Is Ketamine?
Ketamine is a dissociative anaesthetic that modifies neurotransmission in the brain. While it is effective in acute medical settings, its growing use for chronic pain has raised questions about its sustainability and long-term impact.
History and Development
Originally developed in the 1960s as a safer anaesthetic alternative, ketamine became known for its usefulness in acute care. Decades later, its dissociative effects are being explored in mental health and pain management settings, though the evidence remains mixed.
Mechanism of Action
Ketamine blocks NMDA receptors—key components in how your brain interprets and processes pain. By reducing activity in these pathways, ketamine changes your perception of pain, but not the underlying musculoskeletal causes. This disconnect between sensation and dysfunction can lead to inaccurate interpretations of progress or healing.
Ketamine for Pain Management
Ketamine is sometimes used in clinical environments to temporarily reduce severe or treatment-resistant pain. However, most uses in chronic pain management are off-label, and results tend to be short lived.
Low Dose Ketamine Infusion for Postoperative Pain Management
Low-dose ketamine infusion for postoperative pain management can reduce immediate discomfort after surgery. However, postoperative pain and chronic pain are very different scenarios. What works in a controlled, acute environment does not necessarily translate to sustainable, long-term relief.
Benefits and Considerations
Potential Short-Term Benefits
Temporary reduction in pain perception
Helpful in acute surgical situations
May support individuals who cannot tolerate opioid medications
Major Considerations
No strong evidence supports long-term relief
Pain frequently returns once the drug wears off
Potential side effects include dissociation, nausea, dizziness, and cognitive disruption
Interferes with neuromuscular signalling
This last point is especially important for anyone trying to rehabilitate movement patterns.
Why Ketamine (and Pain Medication in General) Can Slow Down Physical Progress
Painkillers, including ketamine, work by dampening the nervous system’s sensitivity to pain signals. While this can provide short-term comfort, there is a hidden cost: Your brain’s ability to accurately sense and coordinate muscle activation becomes impaired.
Human movement is a highly coordinated neuromuscular process. To build better posture, gait mechanics, core integration, and structural balance, your brain must be able to feel what your muscles are doing.
When drugs inhibit pain receptors and alter sensory pathways, it can:
Reduce proprioception
Delay motor learning
Limit the brain’s ability to form stable neuromuscular connections
Mask dysfunctional patterns that still need correcting
Lead to poor technique and compensation during training
In other words: if you can’t accurately sense what your body is doing, you can’t truly fix it.
This is why many people who rely on medication struggle to make long-term progress in movement therapies—they’re training with a muted sensory system.
Why Functional Patterns Offers a More Sustainable Solution
Functional Patterns differs from most pain management approaches because it prioritises root-cause correction through biomechanical re-education. Instead of dulling pain, Functional Patterns focuses on creating:
Better posture
Improved gait cycles
Balanced myofascial tension
Enhanced core mechanics
Reduced joint stress
Efficient force transfer throughout the body
By addressing the structural and neuromuscular imbalances that drive pain, clients experience lasting improvement, often without the need for exogenous substances that interfere with the brain’s signalling.
How Functional Patterns Improves Quality of Life
Functional Patterns training helps your body move the way humans are designed to move—using integrated systems rather than isolated muscles. This leads to:
Consistent reduction in chronic pain
Improved mobility and strength
Better breathing mechanics
Higher energy levels
Increased resilience in daily life
Sustainable progress that builds year after year
Most importantly, results come from within your own body—not from temporary chemical intervention.
Comparison with Other Pain Management Options
While ketamine and other medications may temporarily reduce pain, they do so by altering perception—not fixing dysfunction. This creates a cycle where pain relief becomes dependent on repeated doses, yet movement patterns remain unchanged.
Functional Patterns instead works at the structural level to improve how your body moves, stabilises, and distributes force. This approach corrects the origin of pain rather than suppressing it. Over time, this leads to longer-lasting relief and fewer setbacks.
Lasting Pain Relief Requires Better Movement, Not Stronger Medication
Ketamine may have a place in short-term or emergency pain scenarios, but current research provides no clear evidence supporting its long-term use in chronic pain management. It can reduce sensation, but it cannot repair posture, improve gait, or resolve dysfunctional movement.
To truly overcome chronic pain, you need to improve the way your body functions at a fundamental level. Functional Patterns provides a sustainable, drug-free pathway to pain relief by addressing the structural and neuromuscular causes of discomfort.
Your body has the capacity to heal and perform well—once it learns how to move the way it was designed to.
Sources:
Bell RF, et al. (2018). Ketamine for pain management.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6181464/
Cohen SP, et al. (2018). Consensus guidelines on the use of intravenous ketamine infusions for chronic pain from the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists.
https://rapm.bmj.com/content/rapm/43/5/521.full.pdfCorriger A, et al. (2022). Ketamine for refractory chronic pain: A 1-year follow-up study.
https://journals.lww.com/pain/fulltext/2022/04000/ketamine_for_refractory_chronic_pain__a_1_year.8.aspxCulp C, et al. (2021). Ketamine use for cancer and chronic pain management.
https://www.frontiersin.org/articles/10.3389/fphar.2020.599721/fullFDA approves new nasal spray medication for treatment-resistant depression; available only at a certified doctor’s office or clinic. (2023).
https://www.fda.gov/news-events/press-announcements/fda-approves-new-nasal-spray-medication-treatment-resistant-depression-available-only-certifiedFDA warns patients and health care providers about potential risks associated with compounded ketamine products, including oral formulations, for the treatment of psychiatric disorders. (2023).
https://www.fda.gov/drugs/human-drug-compounding/fda-warns-patients-and-health-care-providers-about-potential-risks-associated-compounded-ketamineKetalar: Ketamine hydrochloric injection. (2022).
https://www.accessdata.fda.gov/spl/data/705c4709-580e-4f02-8a74-bc9aa0641fe2/705c4709-580e-4f02-8a74-bc9aa0641fe2.xmlOrhurhu V, et al. (2019). Ketamine infusions for chronic pain: A systematic review and meta-analysis of randomized controlled trials.
https://journals.lww.com/anesthesia-analgesia/Fulltext/2019/07000/Ketamine_Infusions_for_Chronic_Pain__A_Systematic.40.aspx